Yesterday was my final volunteering shift of the year on the postnatal ward at my local hospital. Each time I go in I spend a few hours visiting with new mums and their babies and it gives me the most amazing opportunity to support women feeding their newborns. Every time I come away having learnt something new, having met more extraordinary women overcome challenges and find confidence in their new role as a Mum. I meet such a huge variety of women – from the really young to the more mature; the first-timer to the Grand Multip with five or more children; the under-privileged to the extremely affluent. And, at the point when I meet them they are totally united by this experience of having given birth. Almost without exception they are instantly catapulted into that maternal need to know that their baby is feeding, is getting what he/she needs and is thriving. The vast majority of women I meet have a desire to breastfeed – they know that their milk is what the baby is expecting to receive, know the benefits for both the baby and themselves, and have possibly even done some classes about feeding. So, why are there problems? And how are we letting women down in this country?
When I was researching an article I wrote for MIDIRS (midwifery) journal earlier this year I read some fairly shocking statistics produced by the Department of Health. In their Indicators of Feeding Quarter 4 2012/2013 report[1] the breastfeeding initiation rate was 73.9% and the prevalence of feeding at 6-8 weeks for the same time period was 47.2%. I have since read further statistics that put the exclusive feeding rate at 6 weeks as 21%. This is shockingly low and begs several questions. Why is the uptake less than ¾ of new mothers? Why is there such a massive decline in breastfeeding in the first few weeks? What experiences are women having and what support are they getting?
In this blog I want to address a few of those questions and I want to put my thoughts about what makes good feeding support out there.
1) Taking Responsibility
For me as a doula, whether it is about the impending birth, parenting choices or feeding options I think taking responsibility is key. And in this instance it is about taking responsibility to educate yourself about what is to come, about asking questions, making informed choices and being aware of options. This is not a time to put your head in the sand. Yes, have an attitude that all will be well because women since time immemorial have fed their babies, but let’s recognize that we don’t exist in the same type of community anymore. We don’t grow up in a village surrounded by women breastfeeding their babies, we often don’t have much to do with babies until we birth our own. Hiring a doula is a positive thing to do – from the research I undertook earlier this year 96.4% of women who gave birth supported by a doula initiated breastfeeding. And of those 586 women, 477 were still exclusively feeding at 6 weeks – 81.4%, a significant difference from the DOH stats I quoted above.
2) Education
This is a tricky one. I meet so many women who took responsibility (see above!), signed up to an antenatal class about feeding and then find that the experience has no bearing on what they learnt. I remember sitting in a, let’s be really honest – profoundly boring, class being shownendless pictures of the anatomy of the breast. And that’s me, someone who is fascinated by the human body, by the ability of a woman to grow life inside her, give birth and then feed her offspring!!! So, what do women need to know when they are educating themselves? Here are just a few of my passionate thoughts!
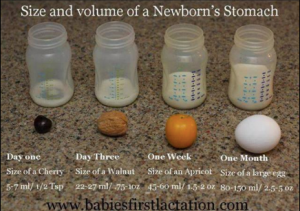
First things first, I want women to know about colostrum – liquid gold as it is sometimes known. That amazing substance that comes from your breasts in the first few days after a baby is born. It comes in small quantities because the baby’s tummy is small, really small, and when I say really small I mean tiny – the size of a small marble. That stuff which contains everything a new baby needs – nutrients, hydration, laxatives to clear the bowel of everything that has been sitting in there whilst the baby was developing in utero, and also the essential ingredients that will strengthen and feed the baby’s microbiome (for anyone interested on that subject a fascinating new film was released this year called Microbirth).
It is possible to hand express colostrum in your late pregnancy and refrigerate or freeze it so that you have some available if there is a need. You won’t run out, it won’t affect how much the baby gets and it can provide peace of mind. Learning how to hand express is an art form – a skill – if you can master it calmly during late pregnancy rather than in the first few days of having a new baby when you are panicking that your precious child hasn’t fed enough then you are on to a winner.
Returning to the size of the baby’s tummy – as I said, it is tiny. So your baby will feed often. We generally say that once the milk comes in, which is around day 3-4, that a baby will expect to feed 8-12 times in 24 hours. But worth knowing that if you have had a caesarean or a medicated or instrumental birth that your baby might go in one of two ways – they may be exceptionally sleepy for a couple of days and not show much interest in feeding at all, OR they might be quite awake, agitated and want to be at the breast a lot. That’s normal. What’s really important is that your breasts be stimulated in those few days, either by your baby, or by hand expressing, as that will be sending the messages to the brain to continue to produce milk. Breastfeeding is supply and demand. The baby can be syringe-fed anything you express out if he/she shows no interest in going to the breast.
Skin to skin. The overwhelming body of evidence about skin to skin makes it a subject worthy of a blog on it’s own (I’ll hold that thought for 2015). However, when it comes to feeding I would prefer to see all babies have uninterrupted skin to skin with their Mum after birth until the first feed is completed, and then as much skin to skin time as is possible in the first few weeks – yes, I said weeks! It is not something that just needs to happen in that golden hour – it is something that will improve the mother-baby connection massively and enables a mum to recognize the early cues that a baby gives far quicker than if the baby is lying on it’s back in a cot, buggy or moses basket. And let’s be honest babies often go from early feeding cue to crying (which is the last resort feeding cue) in a very short space of time! Having skin to skin contact often allows mothers to witness that their baby has the strength, ability and determination to find the breast entirely on his own, without interference. An amazing sight to witness something called the breast crawl (some good Youtube videos on that if you want to see it).
Position and Attachment. The posh terms for latching on. 80% of breastfeeding problems come down to poor position and attachment at the breast. So, for me I want to help women understand what good latching looks like, whilst recognizing that it may vary a bit from woman-to-woman. But, basically to recognize that it is breast-feeding, not nipple-feeding. The important bits for the baby to stimulate are the ducts, which are situated some way back (approximately 3cm) from the nipple. So, we want the nipple, which just contains the tubes through which the milk flows, to be high up and at the back of the baby’s mouth so that it isn’t damaged by tongue or hard palate.
3) Validation
Sometimes all a woman needs to hear is that someone understands. Someone who can say “it sounds like you are having a tricky time” or “given what you have gone through it is not surprising that you feel that way”. It may not seem much, but observing the body language of someone who has been given the opportunity to talk/share/debrief is amazing – the shoulders may drop, the tears may stop, her face may seem clearer, her attitude more positive. It is giving an opportunity for someone to express the fears, concerns, worries, joys etc. Which leads me on to a biggie …
4) Time
This may be the most important. Sadly we know how pushed our maternity services are. We know how few midwives there are and how stretched they are. They don’t have time. What women need more than anything else is for someone experienced to sit with them, listen and observe. They need someone to observe an entire feed, not just the latching on at the start. The perspective of a mother looking down at her baby and breast is very different from someone looking on. Which leads me to my final observation …
5) Qualified Support
The majority of women I meet expect midwives to be able to support them with their feeding. For time reasons already identified that can be problematic, but if we are honest, most midwives do not have enough breastfeeding education during their training. It always shocks people when I say that in some universities midwives only have one day of breastfeeding training in their three year course. One day! I have heard that is changing in some universities across the UK and also as units go for Unicef baby-friendly status, but I find that shocking. And entirely explains why women report getting such conflicting advice from the midwives they encounter on postnatal wards.
So, who can offer qualified support? Firstly, there might be a Feeding Co-ordinator on the ward. So, you could ask to see her when she is on shift. There might be breastfeeding volunteers (like me). All volunteers will have gone through a recognized training – mine was with the Breastfeeding Network as a Peer Helper, with ongoing supervisions with my tutor. There are telephone support lines – the Department of Health has funded an independent line, wo-manned by non-judgemental, trained volunteers (from Breastfeeding Network or Association of Breastfeeding Mothers) – the number is 0300 100 0212 and costs no more than a local call. They are open 0930 -2130 daily. There are free drop-in Breastfeeding support groups – you will find your local groups if you go to either BFN, ABM or La Leche League. They are all run by qualified supporters, who are required to stay up-to-date in their knowledge and practice. The groups/cafes/drop-ins provide a lovely opportunity to meet other mothers, as well as talk to qualified supporters. And, if the need extends beyond the capabilities of any of those, then a Lactation Consultant (IBCLC) – they have had to do hundreds of hours of supervision work, take comprehensive exams etc. Some will also be qualified to perform tongue tie division. http://www.lcgb.org. My go-to Lactation Consultants in SW London are Breastfeeding London
My main point here is to make sure that the support you are getting is qualified and up-to-date. Sadly there are so-called experts out there who are not, and it really saddens me when I hear that yet another mother has stopped breastfeeding because of bad advice and poor support. There is so much research and evidence coming to light all the time – there have been such massive shifts in what we know about feeding in the past ten/twenty/thirty years that no one should be complacent about what they know and how they deliver that information. My commitment is to continue to learn, to spend time with my tutors, to have humility and not to think I know it all. I know that I don’t.